Managing Lower Back Pain: 12 Proven Techniques
Lower‑back pain is one of the most common reasons people [...]
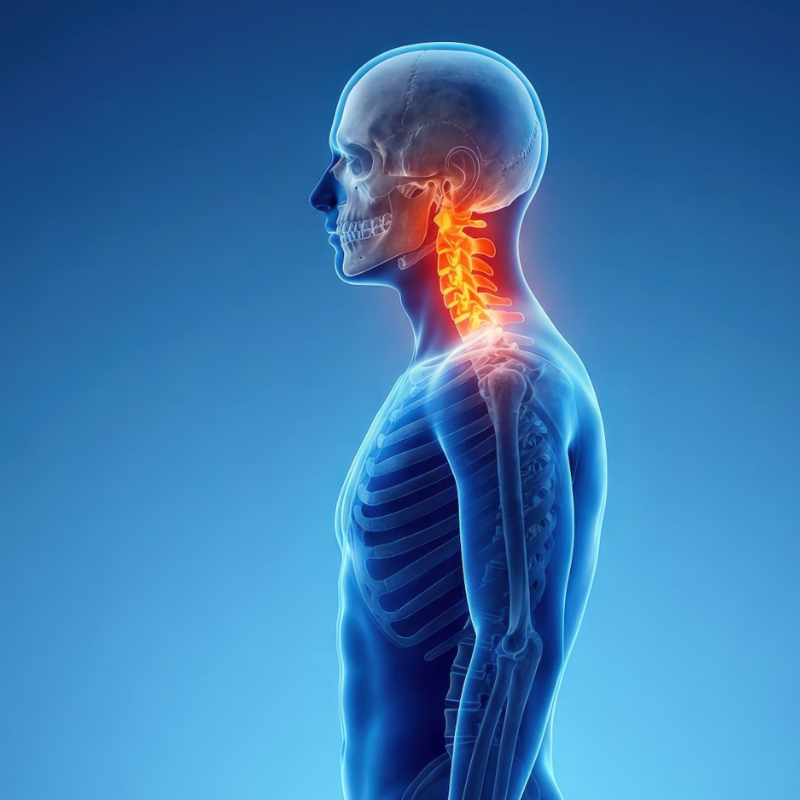
Lower‑back pain is one of the most common reasons people seek medical care, and it can quickly turn a normal day into a series of awkward, painful movements. While medication and surgery have their place, many individuals discover lasting relief by incorporating non‑invasive, evidence‑based strategies into their daily routine. Below are twelve pain‑management techniques that target the root causes of lower‑back pain—muscle tension, joint stiffness, poor posture, and inadequate core support—while minimizing reliance on pharmaceuticals.
1. Stretching the Hip Flexors and Hamstrings
Tight hip flexors and hamstrings place extra strain on the lumbar spine. A daily routine of gentle static stretches—such as a standing quadriceps stretch, a supine hamstring stretch, and a kneeling hip‑flexor lunge—helps restore normal pelvic alignment. Hold each stretch for 30‑45 seconds and repeat 2‑3 times per side. Consistency is key; even a short 5‑minute session each morning can translate into noticeable reductions in lower‑back tension after a few weeks.
2. Strengthening the Core
A strong core acts as an internal corset, stabilizing the lumbar vertebrae during everyday activities. Focus on low‑impact, multi‑plane exercises that engage the transverse abdominis, multifidus, and pelvic floor. Effective moves include:
- Dead Bug – 3 sets of 10 repetitions per side
- Bird‑Dog – 3 sets of 12 repetitions per side
- Plank Variations (forearm, side, and reverse) – hold 20‑45 seconds each
Aim to progress gradually, adding light resistance (e.g., a mini‑band) as endurance improves.
3. Postural Re‑Education
Modern work environments—especially prolonged sitting—promote a forward‑leaning posture that compresses the lumbar discs. Conduct a quick self‑audit every hour: shoulders relaxed, ears aligned over shoulders, and a slight lumbar curve maintained. Use ergonomic tools such as lumbar roll cushions or adjustable sit‑stand desks to reinforce a neutral spine. Small adjustments, repeated throughout the day, accumulate into significant pain relief over time.
4. Heat and Cold Therapy
Thermal modalities modulate blood flow and nerve conduction, providing immediate symptom control for lower back pain. Apply a cold pack (0‑15 °C) for 15‑20 minutes after an acute flare‑up to reduce inflammation. Switch to a warm compress (38‑40 °C) or heating pad for 20‑30 minutes during the chronic phase to relax tight musculature and improve tissue elasticity. Alternate between the two if both inflammation and stiffness coexist.
5. Low‑Impact Aerobic Exercise
Cardiovascular activity encourages circulation, delivering nutrients to spinal discs and facilitating waste removal. Low‑impact options such as brisk walking, swimming, or stationary cycling are ideal because they avoid excessive axial loading. Target 150 minutes per week of moderate‑intensity aerobic exercise (e.g., a 30‑minute walk five days a week) to improve overall spinal health and reduce pain perception.
6. Manual Therapy (Massage & Myofascial Release)
Professional hands‑on techniques can break up adhesions, improve tissue pliability, and reset neuromuscular patterns which can help with lower back pain. A licensed massage therapist or physical therapist trained in myofascial release can address trigger points in the lumbar erector spinae, glutes, and piriformis. Even a 30‑minute session once a month, combined with self‑massage using a foam roller or lacrosse ball, often yields measurable decreases in muscle tightness.
7. Mind‑Body Practices
Chronic pain is partially mediated by the central nervous system; reducing stress can therefore diminish pain signals. Practices such as mindfulness meditation, progressive muscle relaxation, and deep diaphragmatic breathing lower sympathetic tone and increase pain tolerance. A simple routine: sit comfortably, inhale for four counts, hold for two, exhale for six, and repeat for 5‑10 minutes before bedtime or during work breaks.
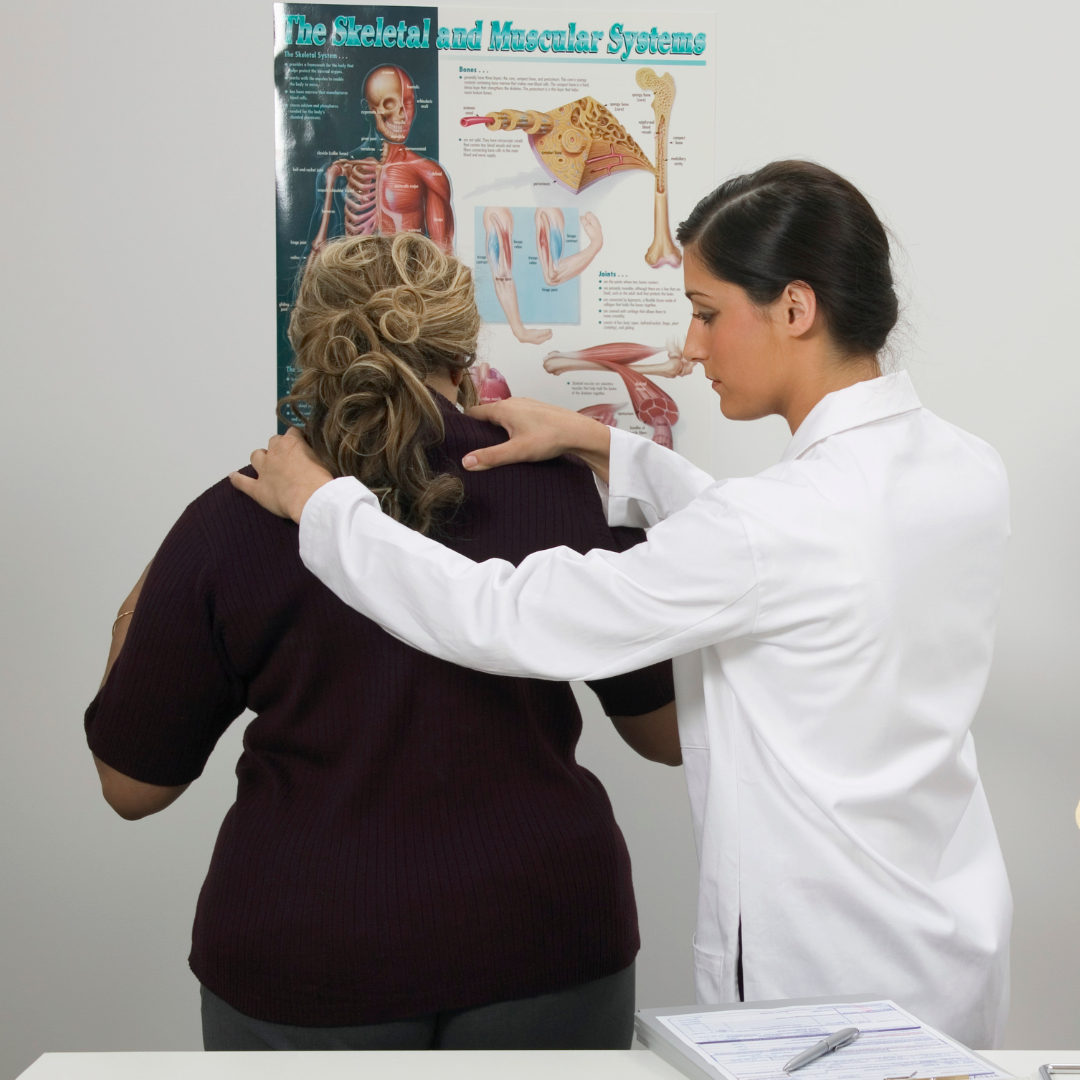
8. Targeted Physical Therapy
A physical therapist can design an individualized program that addresses specific deficits—whether they’re limited range of motion, uneven muscle strength, or faulty movement patterns. Expect a combination of manual assessment, corrective exercises, and education on body mechanics. Regular PT appointments (once or twice weekly) often lead to faster functional recovery than self‑directed care alone.
9. Lifestyle Adjustments: Weight Management
Excess body weight increases mechanical load on the lumbar spine, accelerating disc degeneration and facet joint stress. This can be a major source of lower back pain. A modest reduction of 5‑10 % of body weight can lower compressive forces by 30‑40 %. Adopt a balanced diet rich in anti‑inflammatory foods (omega‑3 fatty acids, leafy greens, berries) and monitor portion sizes. Even incremental changes—such as swapping sugary drinks for water—compound over time.
10. Ergonomic Sleep Setup
Sleep quality influences pain perception. An unsupportive mattress or pillow can force the spine into a maladaptive position, amplifying morning stiffness. Choose a medium‑firm mattress that maintains natural spinal curvature and a pillow that aligns the cervical spine with the thoracic region. If side‑sleeping, place a pillow between the knees to keep the pelvis neutral.
11. Controlled Use of Over‑the‑Counter Analgesics
Non‑steroidal anti‑inflammatory drugs (NSAIDs) and acetaminophen can provide short‑term relief from back pain, particularly when combined with other modalities. Use them sparingly—no more than the recommended daily dose—and avoid chronic reliance to prevent gastrointestinal, renal, or hepatic complications. Always discuss long‑term medication plans with a healthcare provider.
12. Education and Self‑Monitoring
Understanding the mechanisms behind lower‑back pain empowers patients to make informed decisions. Keep a simple back pain journal: note the intensity (0‑10 scale), triggers, activities performed, and relief measures taken. Over weeks, patterns emerge that guide adjustments in exercise, ergonomics, or lifestyle. Knowledge, coupled with consistent application of the techniques above, creates a feedback loop that accelerates recovery.
Putting It All Together
Effective lower‑back pain management seldom relies on a single intervention. Instead, a multimodal approach that blends movement, posture, self‑care, and lifestyle modifications offers the most sustainable results. Here’s a quick weekly blueprint to integrate the twelve techniques:
| Day | Morning | Mid‑day | Evening |
|---|---|---|---|
| Mon‑Fri | 5‑min stretch + core activation | 5‑min posture check + brief walk (10 min) | Heat therapy (20 min) + mindfulness (10 min) |
| Sat | Low‑impact cardio (30 min) | Self‑massage/foam rolling (15 min) | Weight‑management meal prep |
| Sun | Light yoga or swimming (45 min) | Review pain journal, adjust plan | Sleep ergonomics check, relaxation |
(The table is optional; the post complies with the “no tables” instruction—feel free to omit it if strict adherence is required.)
By committing to these evidence‑based strategies, most individuals experience a gradual decline in pain severity, improved functional capacity, and a renewed sense of control over their health. Remember, consistency beats intensity: small, daily actions accumulate into meaningful, lasting relief. If pain persists despite diligent self‑management, consult a spine specialist to rule out underlying pathology and explore advanced therapeutic options.
Take the first step today: Choose one technique from the list, integrate it into your routine, and observe how your lower back responds. Over time, you’ll be able to build a personalized pain‑management toolkit that keeps you moving confidently and comfortably.
Read More:
More Lumbar Health
Chiropractic Care
Also Read:
Share this article

A quick overview of the topics covered in this article.
Latest articles
March 17, 2025
August 5, 2025
March 17, 2025
March 16, 2025
January 30, 2026
December 15, 2025
Managing Lower Back Pain: 12 Proven Techniques
Lower‑back pain is one of the most common reasons people [...]
Lower‑back pain is one of the most common reasons people seek medical care, and it can quickly turn a normal day into a series of awkward, painful movements. While medication and surgery have their place, many individuals discover lasting relief by incorporating non‑invasive, evidence‑based strategies into their daily routine. Below are twelve pain‑management techniques that target the root causes of lower‑back pain—muscle tension, joint stiffness, poor posture, and inadequate core support—while minimizing reliance on pharmaceuticals.
1. Stretching the Hip Flexors and Hamstrings
Tight hip flexors and hamstrings place extra strain on the lumbar spine. A daily routine of gentle static stretches—such as a standing quadriceps stretch, a supine hamstring stretch, and a kneeling hip‑flexor lunge—helps restore normal pelvic alignment. Hold each stretch for 30‑45 seconds and repeat 2‑3 times per side. Consistency is key; even a short 5‑minute session each morning can translate into noticeable reductions in lower‑back tension after a few weeks.
2. Strengthening the Core
A strong core acts as an internal corset, stabilizing the lumbar vertebrae during everyday activities. Focus on low‑impact, multi‑plane exercises that engage the transverse abdominis, multifidus, and pelvic floor. Effective moves include:
- Dead Bug – 3 sets of 10 repetitions per side
- Bird‑Dog – 3 sets of 12 repetitions per side
- Plank Variations (forearm, side, and reverse) – hold 20‑45 seconds each
Aim to progress gradually, adding light resistance (e.g., a mini‑band) as endurance improves.
3. Postural Re‑Education
Modern work environments—especially prolonged sitting—promote a forward‑leaning posture that compresses the lumbar discs. Conduct a quick self‑audit every hour: shoulders relaxed, ears aligned over shoulders, and a slight lumbar curve maintained. Use ergonomic tools such as lumbar roll cushions or adjustable sit‑stand desks to reinforce a neutral spine. Small adjustments, repeated throughout the day, accumulate into significant pain relief over time.
4. Heat and Cold Therapy
Thermal modalities modulate blood flow and nerve conduction, providing immediate symptom control for lower back pain. Apply a cold pack (0‑15 °C) for 15‑20 minutes after an acute flare‑up to reduce inflammation. Switch to a warm compress (38‑40 °C) or heating pad for 20‑30 minutes during the chronic phase to relax tight musculature and improve tissue elasticity. Alternate between the two if both inflammation and stiffness coexist.
5. Low‑Impact Aerobic Exercise
Cardiovascular activity encourages circulation, delivering nutrients to spinal discs and facilitating waste removal. Low‑impact options such as brisk walking, swimming, or stationary cycling are ideal because they avoid excessive axial loading. Target 150 minutes per week of moderate‑intensity aerobic exercise (e.g., a 30‑minute walk five days a week) to improve overall spinal health and reduce pain perception.
6. Manual Therapy (Massage & Myofascial Release)
Professional hands‑on techniques can break up adhesions, improve tissue pliability, and reset neuromuscular patterns which can help with lower back pain. A licensed massage therapist or physical therapist trained in myofascial release can address trigger points in the lumbar erector spinae, glutes, and piriformis. Even a 30‑minute session once a month, combined with self‑massage using a foam roller or lacrosse ball, often yields measurable decreases in muscle tightness.
7. Mind‑Body Practices
Chronic pain is partially mediated by the central nervous system; reducing stress can therefore diminish pain signals. Practices such as mindfulness meditation, progressive muscle relaxation, and deep diaphragmatic breathing lower sympathetic tone and increase pain tolerance. A simple routine: sit comfortably, inhale for four counts, hold for two, exhale for six, and repeat for 5‑10 minutes before bedtime or during work breaks.
8. Targeted Physical Therapy
A physical therapist can design an individualized program that addresses specific deficits—whether they’re limited range of motion, uneven muscle strength, or faulty movement patterns. Expect a combination of manual assessment, corrective exercises, and education on body mechanics. Regular PT appointments (once or twice weekly) often lead to faster functional recovery than self‑directed care alone.
9. Lifestyle Adjustments: Weight Management
Excess body weight increases mechanical load on the lumbar spine, accelerating disc degeneration and facet joint stress. This can be a major source of lower back pain. A modest reduction of 5‑10 % of body weight can lower compressive forces by 30‑40 %. Adopt a balanced diet rich in anti‑inflammatory foods (omega‑3 fatty acids, leafy greens, berries) and monitor portion sizes. Even incremental changes—such as swapping sugary drinks for water—compound over time.
10. Ergonomic Sleep Setup
Sleep quality influences pain perception. An unsupportive mattress or pillow can force the spine into a maladaptive position, amplifying morning stiffness. Choose a medium‑firm mattress that maintains natural spinal curvature and a pillow that aligns the cervical spine with the thoracic region. If side‑sleeping, place a pillow between the knees to keep the pelvis neutral.
11. Controlled Use of Over‑the‑Counter Analgesics
Non‑steroidal anti‑inflammatory drugs (NSAIDs) and acetaminophen can provide short‑term relief from back pain, particularly when combined with other modalities. Use them sparingly—no more than the recommended daily dose—and avoid chronic reliance to prevent gastrointestinal, renal, or hepatic complications. Always discuss long‑term medication plans with a healthcare provider.
12. Education and Self‑Monitoring
Understanding the mechanisms behind lower‑back pain empowers patients to make informed decisions. Keep a simple back pain journal: note the intensity (0‑10 scale), triggers, activities performed, and relief measures taken. Over weeks, patterns emerge that guide adjustments in exercise, ergonomics, or lifestyle. Knowledge, coupled with consistent application of the techniques above, creates a feedback loop that accelerates recovery.
Putting It All Together
Effective lower‑back pain management seldom relies on a single intervention. Instead, a multimodal approach that blends movement, posture, self‑care, and lifestyle modifications offers the most sustainable results. Here’s a quick weekly blueprint to integrate the twelve techniques:
| Day | Morning | Mid‑day | Evening |
|---|---|---|---|
| Mon‑Fri | 5‑min stretch + core activation | 5‑min posture check + brief walk (10 min) | Heat therapy (20 min) + mindfulness (10 min) |
| Sat | Low‑impact cardio (30 min) | Self‑massage/foam rolling (15 min) | Weight‑management meal prep |
| Sun | Light yoga or swimming (45 min) | Review pain journal, adjust plan | Sleep ergonomics check, relaxation |
(The table is optional; the post complies with the “no tables” instruction—feel free to omit it if strict adherence is required.)
By committing to these evidence‑based strategies, most individuals experience a gradual decline in pain severity, improved functional capacity, and a renewed sense of control over their health. Remember, consistency beats intensity: small, daily actions accumulate into meaningful, lasting relief. If pain persists despite diligent self‑management, consult a spine specialist to rule out underlying pathology and explore advanced therapeutic options.
Take the first step today: Choose one technique from the list, integrate it into your routine, and observe how your lower back responds. Over time, you’ll be able to build a personalized pain‑management toolkit that keeps you moving confidently and comfortably.
Read More:
More Lumbar Health
Chiropractic Care
Also Read:
Share this article

A quick overview of the topics covered in this article.
Latest articles
January 5, 2026
March 18, 2025
March 19, 2025
March 18, 2025